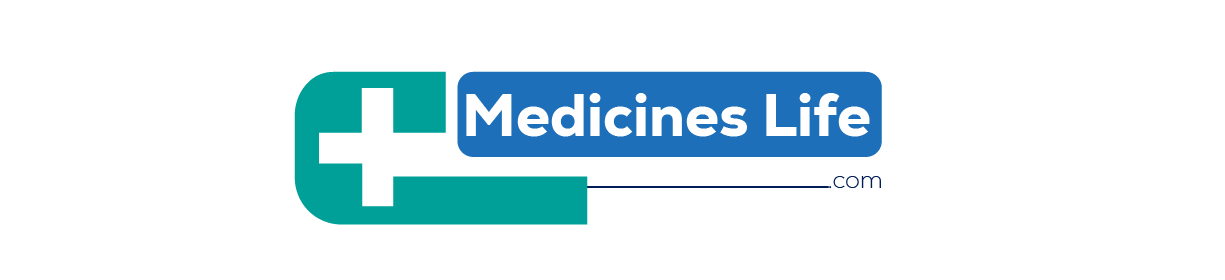
Asthma
Chronic asthma is a respiratory disease that causes inflammation and airway narrowing, which makes breathing difficult and causes wheezing, coughing, and shortness of breath. It can be minor or severe, and it affects people of all ages. Exercise, stress, allergies, and respiratory infections are all common causes of asthma. Medication, symptom monitoring, and avoiding triggers are all necessary for effective management.
Types of Asthma

Allergic Asthma
- Caused by allergens like mold, dust mites, pollen, and pet dander.
- Frequently linked to additional allergy diseases such as allergic rhinitis and eczema.

Non-Allergic Asthma
- Other than allergens, such as cold air, exercise, stress, and respiratory illnesses, cause the reaction.
- With the exception of the allergy component, symptoms resemble those of allergic asthma.

Occupational Asthma
- Caused by being around irritating substances at work, like dust, fumes, or chemicals.
- When away from the workplace, symptoms get better.

Exercise-Induced Asthma (EIA)
- Usually manifests during or after strenuous activity, particularly in chilly or dry environments.

Childhood Asthma
- Often diagnosed in childhood.
- Usually happens during or after exercise. Induced by physical activity, especially in cold or dry air.

Adult-Onset Asthma
- Occurs in adults and frequently does not have a history of asthma.
- May be brought on by work hazards or respiratory illnesses.
Symptoms
- Breathlessness
- wheezing, or making a whistling noise when breathing
- Coughing, particularly in the early morning or at night
- Pain or tightness in the chest
- increased mucus production
- breathing issues preventing you from falling asleep

Causes
- Genetics: A family history of allergy disorders, including asthma.
- Environmental factors include exposure to tobacco smoke, pollution, and allergens such as pollen, dust mites, pet dander, and mold.
- Infections of the respiratory system: Viral infections, particularly in early childhood, can raise the chance of developing asthma.
- Workplace exposures include chemicals, dust, and fumes.
- Exercise: Especially outside in the cold or dry air.
- Stress: The symptoms of asthma can be brought on by emotional stress and anxiety.
Risk Factors
- Family History: The chance of having asthma is largely influenced by genetics.
- Allergies: Having additional allergic reactions, such as rhinitis or eczema.
- Asthma risk is increased in obesity.
- Smoking: Both active and passive exposure to tobacco smoke.
- Exposure to elevated amounts of environmental contamination.
- Occupational Exposures: Specific occupations where there is a risk of irritation.
Diagnosis
Medical History and Physical Examination: Comprehensive symptom history, family medical history, and respiratory system examination.
Lung Function Tests:
Spirometry: determines how much air a somebody can exhale quickly after taking a deep breath.
Peak Flow Meter: a basic instrument to assess the fastest possible exhalation rate.
Allergy Testing: Tests on the skin or blood to pinpoint certain allergies.
Methacholine Challenge Test: Inhaling a material that constricts the airways; if lung function tests are normal, this is used to identify asthma.
Exhaled Nitric Oxide Test: Determines the level of nitric oxide in the breath, which is a sign of lung inflammation.

Medications
Long-Term Control Medications:
- Inhaled Corticosteroids: Fluticasone (Flovent), budesonide (Pulmicort) to reduce inflammation.
- Long-Acting Beta Agonists (LABAs): Salmeterol (Serevent), formoterol (Foradil) to open airways.
- Leukotriene Modifiers: Montelukast (Singulair), zafirlukast (Accolate) to block inflammatory chemicals.
- Combination Inhalers: Contain both inhaled corticosteroids and LABAs (Advair, Symbicort).
- Theophylline: A bronchodilator used for long-term control.
Quick-Relief Medications:
Short-Acting Beta Agonists (SABAs): Albuterol (ProAir, Ventolin), levalbuterol (Xopenex) for rapid relief of symptoms.
Anticholinergics: Ipratropium (Atrovent) to relax airways.
Oral and Intravenous Corticosteroids: Prednisone, methylprednisolone for severe asthma attacks.
Biologic Therapies:
Omalizumab (Xolair): For severe allergic asthma, targets IgE antibodies.
Mepolizumab (Nucala), Reslizumab (Cinqair), Benralizumab (Fasenra): Target interleukins involved in the inflammatory response.

Non-Medication Treatments:
- Breathing exercises: Methods to enhance lung function, such as diaphragmatic and pursed-lip breathing.
- A program called pulmonary rehabilitation helps patients manage their illness by providing them with education, support, and instruction in exercise.
- Managing allergies involves staying away from recognized allergens and employing allergy medications like immunotherapy (allergy injections).
Prevention
- Eliminate Triggers: Recognize and steer clear of allergens and irritants that exacerbate symptoms.
- Control the environment by using air filters, lowering indoor humidity, avoiding tobacco smoke, and reducing dust mites.
- Frequent Monitoring: To keep an eye on lung health and spot early warning indicators of an attack, use a peak flow meter.
- A healthy lifestyle entails eating a balanced food, doing regular exercise, and maintaining a healthy weight.
- Vaccinations: To avoid respiratory illnesses, get vaccinated against pneumonia and influenza.

Complications
- Asthma Attacks: Severe flare-ups necessitating immediate medical attention.
- Increased vulnerability to infections such as bronchitis and pneumonia is known as a respiratory illness.
- Permanent Airway Remodeling: Prolonged inflammation might cause the airways to permanently remodel, which will lower lung function.
- Psychological Impact: Stress and anxiety brought on by managing a chronic illness.
Pharmacist Interventions
- Medication counseling: Inform patients on how to use inhalers correctly, how to follow their prescription schedules, and how to handle side effects.
- Asthma Action strategy Development: Assist patients in developing a customized strategy that outlines how to identify and address exacerbating symptoms.
- Symptom Monitoring: Instruct patients on how to track their status by recording symptoms and using peak flow meters.
- Identification and Avoidance of Triggers: Offer advice on locating and steering clear of asthma triggers.
- Support and Education: To assist patients in managing their disease, provide support groups and educational materials.
Conclusion
Asthma is a chronic but treatable illness that calls for a multifaceted strategy that includes medicine, lifestyle changes, and ongoing observation. Having a better understanding of the many forms of asthma, as well as its causes, symptoms, and therapies, can help people manage their illness and enhance their quality of life. When asthma symptoms are severe or persistent, always seek medical advice.